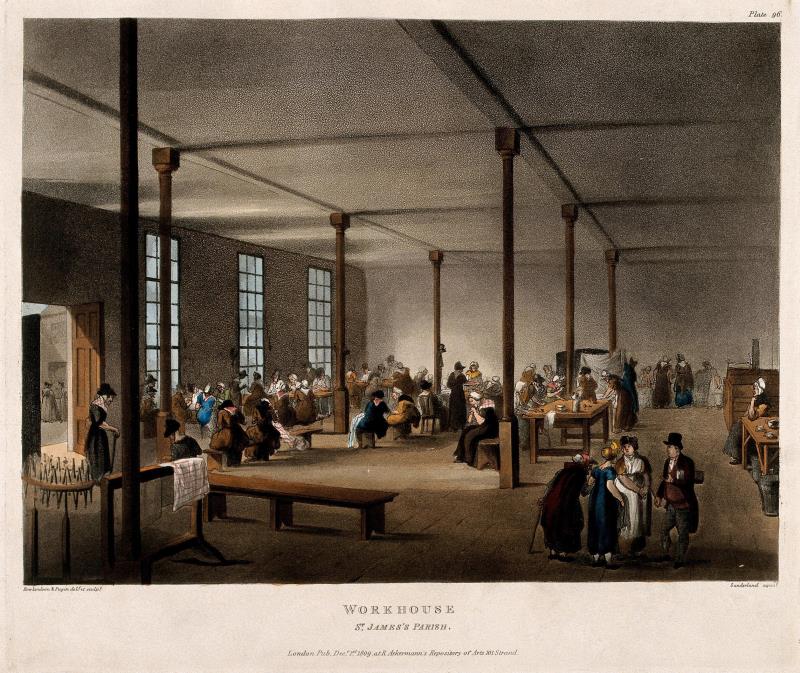
Increased life expectancy is certainly a positive development. Older
people are more connected, active for longer, and find support in
technologies from Skype to stair lifts and digital companions. Yet age
discrimination still exists and society continues to view older age as a problem.
Around the UK, nursing initiatives are taking place to address how we
care for older people. These can be small interventions like anti-spill mugs
and easy grip cutlery, to wearable ‘smart’ glasses which enable care
workers to live stream to other professionals for advice and diagnoses.
But innovation isn’t just about new technologies. It’s about ensuring
better communication and having skilled practitioners in place at the
right time. In 2016, Burton Hospitals NHS Foundation Trust introduced
a dedicated service of health care assistants specially recruited to work
with older people. Assistants gave one to one support to the same
patient for as long as care was needed, enabling them to build trust and
a relationship with that person. It meant fewer doctor call-outs and next
to no patient falls.
It is members of the nursing family who are best placed to ensure their
patients, whether in their own home or a care home, achieve a sense of
security, belonging and purpose.

![Four specimens of sea skink, late eighteenth century. On loan from the Royal Pharmaceutical Society. Believed to be an aphrodisiac, sea skink was reported to ‘restore warmth in old age [and] decays of nature’ and increase ‘the Semen Virile’.](https://www.rcn.org.uk/library-exhibitions/-/media/Royal-College-Of-Nursing/Images/Library-exhibitions/Aspects-of-age/Image-gallery/Sea-skink.JPG)