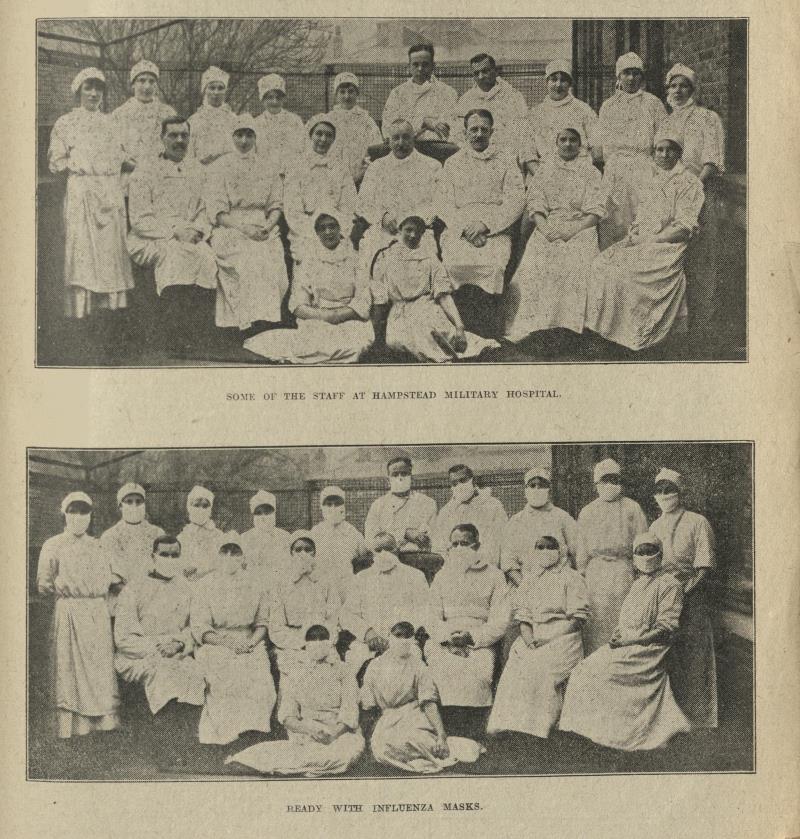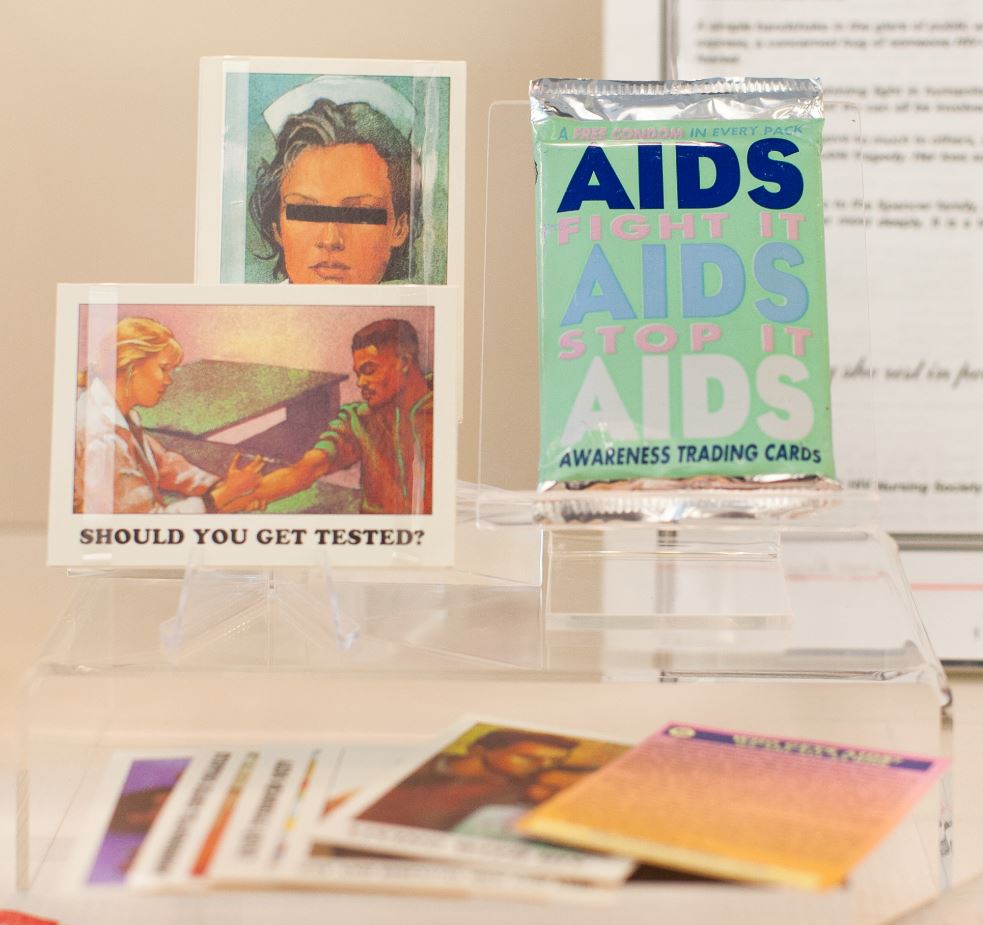
Personal protective equipment, or PPE, has become a household term in 2020. Images of masked medics and robed nurses have been made all too familiar by the media in recent years. News reporting on the Ebola outbreak in 2014 is a key example of this. The Lassa Fever hospital in Kenema, Sierra Leone, was one of the first in the country hit by the Ebola virus. In just a few short months, the clinic lost 15 nurses to the disease.
To those outside Ebola affected countries, the current climate makes it easy to forget that Ebola outbreaks are still happening. More recent cases in the Democratic Republic of Congo’s Equateur province continue to be a concern. Responding to Ebola within the COVID-19 context is a huge challenge. UK nurses and health care teams continue to support local communities in Ebola prevention and health care maintenance.
"Today I woke up with a cold, a surprising thing given how many hundreds of times a day I wash my hands with chlorine to kill Ebola. Chlorine is the bullet that kills the enemy we can’t see."