Search
You are currently searching within the context of the global site
Search in local site-
Amplifying the voices of Arab nurses

The British Arab Nursing and Midwifery Association (BANMA) is providing support to professionals while advocating for improved health care in the British Arab community.
-
Collaborating with police on mental health care

How nursing staff and police can work together to improve mental health provisions
-
Meet the NHS’s first Filipino CNO: ‘I hope people see me and realise they can do it too’

More than 25,000 nurses who are educated in the Philippines work in the NHS, but Oliver Soriano is the first to make it to the top.
-
Nursing voices of the Windrush generation
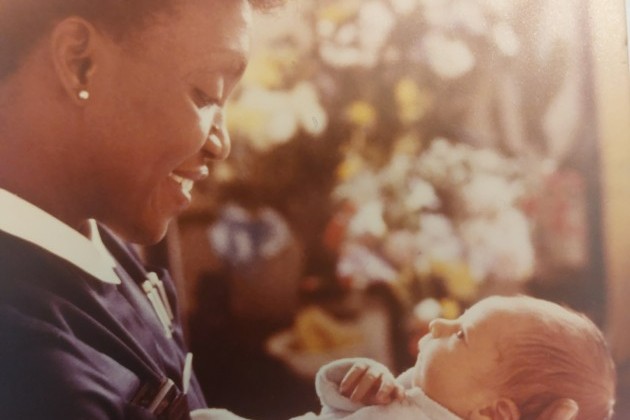
‘We mustn’t forget their struggles, and that some of those struggles continue’. Many of the people who arrived in the UK from the Caribbean in 1948 became instrumental in the development of the NHS. We share the stories of four nurses who’ve been involved with or touched by the Windrush legacy
-
Video: 'When I was homeless I wasn't able to work – now I'm back helping patients'

Find out how the RCN Foundation helped Lily and her family get back on their feet, so they can look forward to a safe and stable Christmas together this year
-
The Soho clinic spearheading LGBTQ+ health care

Clinic manager Jon Clark from Soho sexual health clinic 56 Dean Street talks about the importance of the clinic's work to the LGBTQ+ community.
-
Wellbeing

Read the latest RCN Magazine articles here
-
In conversation: living with and beyond suicidal thoughts

Nurses Liz and Shelley talk about their experiences of suicidal ideation, seeking help and supporting others
-
How to wind down to sleep

It’s not always easy to switch off and get a good night’s sleep, but it’s essential for wellbeing. Find out how you can you aid better sleep and what to do if you’re struggling to nod off at night.
-
Five ways to combat compassion fatigue

Five ways to combat compassion fatigue






