Following two weeks of annual leave being a mum to my curious two-year-old, I was worried about returning to work. In my time off, I read a lot about the issues with the supply of personal protective equipment (PPE), how my nursing colleagues have been falling sick in hospitals and communities around the world, and the frightening daily death tolls due to COVID-19.
I knew my workplace wouldn’t be the same, nor would I be doing the role I once had. I was anxious about how my husband would be able to work from home while looking after my little boy and how I would manage the lengthy journey to work with disrupted public transport.
I also worried about my ability to work with intubated patients in an intensive care setting. The night before my first shift I had nightmares about feeling suffocated wearing PPE. In spite of all these anxieties, a part of me wanted to face my fears and experience the reality for myself.
Before my first shift I had nightmares about feeling suffocated wearing PPE
On my first day back, I was redeployed to work in a COVID-19 intensive care unit. The entire hospital had changed to be able to deal with the pandemic. While I’d heard some horror stories, at my trust the strategic planning was very impressive. All our PPE was displayed neatly, and I felt reassured that I was supported and looked after.
Stepping into the ITU, I realised things had completely altered. What was a cardiothoracic high dependency unit two weeks ago was now a full to the brim COVID-19 intensive care unit, with every patient critically ill and being supported on a ventilator.
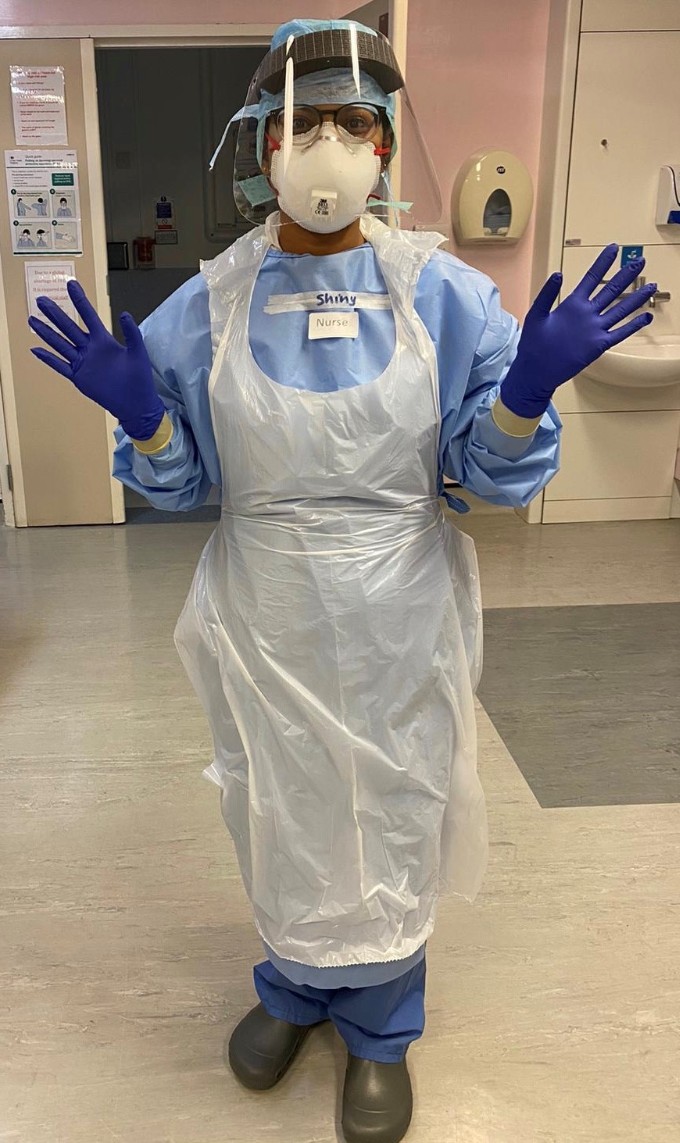
I was surprised to see so many younger patients in their 30s to 50s, many with no significant underlying health issues. All staff had to wear a surgical hat, a visor, goggles, a full body long-sleeved gown, plastic apron and double gloves. No personal belongings, mobile phones or drinks were allowed. Every available space, including the toilets, was being used to store equipment.
This was my first shift in two years when I’d had to deal with ventilators and many of us were in a similar situation. As I worked alongside a paediatric intensive care nurse, I could feel her emotions. Cardiologists and surgeons were inserting central lines, vascaths for renal filtration and arterial lines - procedures usually performed by an anaesthetic team. Working out of our comfort zones was nerve-wracking, the impact compounded by a new disease and critically ill patients.
All of us were sweating inside our PPE, with the strap from the mask hurting my ears and my nose bridge getting sore. We couldn’t go for a quick toilet break or even recognise each other with our full gear on, as we were forced to speak loudly to be heard through the masks.
Medication was running lower than it did for a month in normal circumstances. Patients were relying on our management, while their families, not allowed to visit their loved ones, were crying over the phone as they tried to get updates.
This was my harsh reality on just my first day, with many more to come.








