Skin cancer is now one of the most common cancers in the UK, and it’s on the rise.
In the last decade, rates of melanoma skin cancer in particular have increased by 31% in Britain, resulting in an average of 48 people being diagnosed every day. By 2038-2040, it’s estimated there could be around 26,500 new cases of melanoma skin cancer every year in the UK.
While there are specialist dermatology nurses who support patients with diagnosis and treatment, nursing staff are often the first to spot skin changes in their patients.
“All nursing staff have a role to play in identifying moles and lesions that look suspicious, and escalating any concerns to ensure safe care for their patients,” says Callum Metcalfe-O'Shea, RCN Professional Lead for Long-Term Conditions.
From how to assess moles and lesions to understanding next steps if you identify an abnormality, read on to find out what you need to know. Or watch our video on how to use the ABCDE approach.
The ABCDE approach
One of the most useful tools that all nursing staff can use to help assess moles and skin lesions is the ABCDE approach.
This structured approach uses five simple steps to identify any signs of possible melanoma or potential for further investigation.
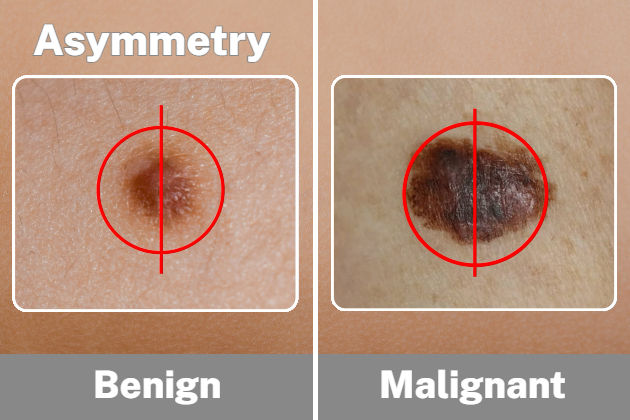
A – asymmetry
Normal moles will appear symmetrical (both halves will look the same). However, melanomas are likely to be irregular and asymmetrical.
B – border
Normal moles will have a well-defined border that is smooth and clear to see, but melanomas are more likely to have irregular, blurred or jagged edges.

C – colour
Normal moles will usually be one shade of colour. Melanomas tend to be more than one colour and can be mixed with shades of brown, red, pink, blue or white.

D – dimension
Normal moles are not usually bigger than the blunt end of a pencil, whereas melanomas are usually more than 6mm wide.

E – evolution/everything else
If a mole becomes larger or darker, or starts to ooze, itch or become crusty – a review may be required.

Assessing darker skin tones
Skin cancer and melanoma affect all skin types, including people with black and brown skin, but it can be more difficult to spot.
Tracy Paine MBE, registered nurse and CEO of Melanoma UK, says: "Melanomas in skin of colour can be challenging to identify due to the masking effect of surrounding skin. Photographic surveillance, including total body photography, and dermoscopy, can really help to improve detection.”

Acral melanoma is a rare form of skin cancer, but it’s most common in the Global Majority. Tracy advises that it’s important to look out for irregular shape, colour and size changes, including:
- a new streak in a nail that is not caused by an accident or bruise
- a nail streak that has damaged the fingernail
- a changing spot that's in, or connected to, a mole on the foot or hand
- an irregularly shaped growth on the foot or hand that is changing, growing or has an unusual colour
- an elevated, thickened patch which is growing on the sole of the foot or palm of the hand.
Next steps
If you’ve identified a mole or lesion that looks different and needs further assessment, these are the key principles you need to follow.
- Document clearly: using the ABCDE approach. Note the site, size and duration of the mole. Where possible, use skin maps/templates to identify exactly where on the body the mole of concern is located.
- Take photography: taking a digital image is useful for referral and for identifying if changes occur at a later period. Make sure you follow your local policy around consent.
- Undertake dermoscopy: at advanced levels, nurses may be trained to undertake dermoscopy to review a mole in more depth. Using a specific magnifying tool (dermatoscope), trained nurses can view the area at 10 times the size, to consider any cellular changes that may require prompt referral.
- Know your referral pathways: depending on the clinical setting and referral pathways, nursing staff (usually at enhanced or advanced levels) may be able to refer patients for specialist input via a dermatology department.
If in doubt, or if you don’t have access to these pathways, advise your patients to arrange a prompt appointment at their GP practice for further review.
It’s important to note that although skin cancer and melanoma is rare in children and adolescents, it can occur. Callum advises that nursing staff caring for children and adolescents will need to follow the same principles detailed above.
Finding opportunities
Early detection can mean early treatment, and almost everyone with stage 1 melanoma skin cancer will survive their cancer for five years or more after diagnosis.
“Nursing staff are in a unique position. Working in close proximity to patients and their skin means nursing staff can get involved to either identify, escalate, refer on, or support skin cancer treatment,” says Callum.
Read next: How to perform a diabetic foot check
Callum urges all nursing staff to think about the setting they work in and how they can they can support early detection.
Here are just a few suggestions for some common work places.
- Care homes: when washing, dressing and providing continence care.
- Prisons: when providing health assessments and wound care.
- Hospitals: when carrying out admission assessments or pressure ulcer checks.
- Primary care: when conducting chronic disease reviews and wound care.
- Social care: when delivering personal care, care planning visits, or when moving and handling.
- Community: on district nurse visits, when providing catheter care, wound care, or skin integrity assessments.
In every nursing role, there’ll be opportunities to examine and inspect a patient’s skin for abnormalities that may require further investigation. Here’s how you can support your patients within your role and your level of nursing:
- Supportive (eg HCSW or HCA): escalate any incidence to the registered nurse for review and document accordingly on patient records or skin maps/templates.
- Assistive (eg nursing associate): escalate any incidence to the registered nurse and document accordingly on patient records or skin maps/templates, signpost to relevant health information leaflets or sites for further support.
- Registered / enhanced: (eg staff nurse, practice nurse, community nurse, care home nurse, prison nurse): document any changes accordingly on patient records or skin maps/templates, assess for any other concerning symptoms and check for any other concerning lesions, refer to advanced or consultant level.
- Advanced (eg advanced nurse practitioner, advanced clinical practitioner): if trained, undertake dermatoscope investigation, assess for any systemic involvement such as fever, weight loss, metastases, etc; and refer via your local pathway for suspected skin cancer.
- Consultant (eg consultant nurse, consultant skin cancer nurse specialist): provide expert advice and treatment autonomously, including prescribing and where required, surgical treatment.
Action points
“All nursing staff can increase their awareness and knowledge of what skin changes may require further investigation,” Callum says.
Here are some actions you can take into your clinical setting, right away.
- Download posters and leaflets
Download leaflets and posters free of charge from the the British Association of Dermatologists. These can be extremely useful to help staff and patients to recognise when a mole may be changing or could be a concern. - Create checklists
Use the ABCDE approach within your clinical area to create a checklist approach for any mole or lesion you identify as concerning. - Use measuring tools
Promote the use of measuring tools (such as infection control-friendly rulers/measuring tapes) to help identify any moles of concern, or review if a mole is changing or growing. - Identify escalation pathways
Work with your clinical leadership team to identify what pathways may be needed to help nursing staff, of all levels, recognise how they can escalate any concerns around mole changes.
Further information
If you'd like to find out more about performing mole checks or to access resources to support your patients and colleagues, you can visit the Melanoma UK and NHS websites.








