Our new resources help you look after your skin and seek support to prevent long-term damage to your hands
The COVID-19 pandemic began with instructions for everyone to wash their hands. Nursing staff always pay close attention to hand hygiene, but with handwashing, alcohol rub and gloves being used more frequently than usual, your skin could be suffering.
A recent RCN survey found that 93% of nursing staff had experienced some form of skin condition, including dryness, redness, cracking, itching and pain, in the previous year.
We’ve now launched a new set of resources to help you look after your skin health.
There’s advice on hand hygiene, glove use and when to seek support. There’s also an online learning module about the skin condition dermatitis.
“The COVID-19 crisis has thrown light on the importance of protective equipment for nursing staff in keeping them and their patients safe,” says Rose Gallagher, RCN Professional Lead for Infection Prevention and Control.
“When there is regular, prolonged use of this protective equipment, including gloves, nursing staff need to continue to take care of their skin health to prevent long-term damage.”

Hand health
Nursing staff come into contact with lots of irritants at work, which could cause hand health issues.
The RCN survey revealed that dryness is the most common symptom, with 90% of respondents experiencing dry hands. Alongside this, around two-thirds of people experienced redness, itching and cracking of the skin.
These can all be signs of dermatitis, the main work-related skin condition affecting the hands of nursing staff. Infection prevention and control measures, such as handwashing, alcohol gel and glove use can all cause or worsen dermatitis.
Meanwhile, damaged skin can prevent effective hand hygiene, so it’s extra important to check for signs while working during the COVID-19 pandemic.
If you’re experiencing any of these symptoms, you should seek help and advice from your occupational health service or your GP.
Kim Sunley, RCN National Officer, says: “Employers have a legal duty to assess and take measures to protect staff from developing work-related skin conditions. If your skin is damaged, you should file an incident report, so that your employer is made aware of the volume of skin health issues and can take steps to deal with this.
"We would also expect employers to provide hand moisturisers containing emollients for nursing staff to access at work."

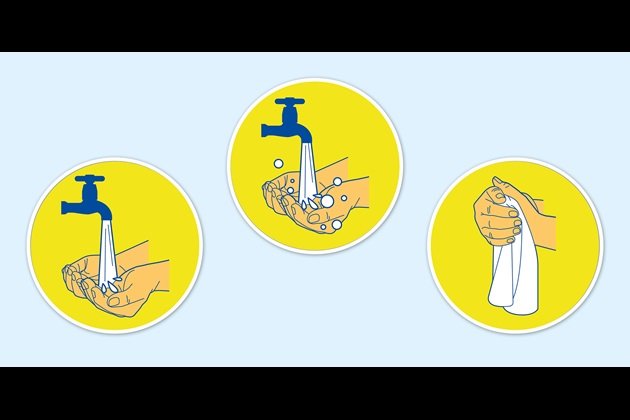
Top tips for hand health
- Always wet hands thoroughly before applying soap.
- Rinse off all soap when washing hands.
- Dry hands thoroughly after washing – pat skin with a soft paper towel where possible and avoid hand dryers if you can.
- Apply moisturiser containing emollient to hands regularly.
- Stay hydrated.
- Gloves are not a substitute for hand hygiene. Over-use can put you at risk of dermatitis.
Be glove aware
“We know that, even in normal times, far too often gloves are worn when they’re not necessary,” says Rose. “This can have a real impact on skin health, even forcing some to change their jobs. In the current circumstances we are all being extra vigilant about hygiene, but using gloves should not be seen as a replacement for good hand hygiene.”
Using gloves should not be seen as a replacement for good hand hygiene
It is important to assess when to use gloves and avoid unnecessary use as much as possible, as both under and overuse of gloves can put you at risk of dermatitis. Gloves should be worn if you’re in contact with blood, body fluid, broken skin, or mucous membranes. They’re also needed if there’s a chance of chemical hazards such as disinfectants or cytotoxic drugs touching your hands.
You should only put gloves on when your hands are completely dry. And you should remove gloves when the task that required them is complete – remember, gloves are single-use items so they should be removed and changed between each patient or care task.

Skin safety while using PPE
During the COVID-19 pandemic, you may be using other forms of PPE too, such as gowns, overalls, eye protection and face masks.
There have been many images in the media of health care workers whose face has been marked by long shifts wearing face masks. As with the skin on your hands, broken skin elsewhere on your body can be an infection risk.
Public Health England recommends only wearing PPE for two-hour stretches, so that your skin can dry and recover. Having regular breaks will also allow you to rehydrate by drinking water, and by applying moisturiser containing emollients to the pressure points where your PPE touches your skin.
Masks that have been fit tested are less likely to damage your skin. Even if you have been fit tested, check your skin regularly for any signs of redness, soreness or cracking. If you spot any, report this to your line manager and occupational health.
Read our full guidance on maintaining skin health while using PPE.
Remember and report
Under health and safety law, your employer should have a programme of skin checks in place for nursing staff exposed to the risk of work-related dermatitis. Report any problems to your manager or occupational health provider. If you need further support, contact your local RCN safety rep or call RCN Direct on 0345 772 6100.
Skin health resources
Our full set of skin health resources are available here.
The resources have been created in collaboration with Mölnlycke and SC Johnson Professional.