Staff shortages are threatening the quality of patient care, with nurse vacancies reaching new heights. But as Wales and Scotland look to the law to address the problem, RCN Bulletin considers what progress has been made
Last year, when the RCN asked nursing staff to describe their last shift, responses flooded in – 30,000 in just two weeks.
Some time has passed since that survey in May but revisiting respondents’ comments has done little to diminish their power.
“I drove home from work sobbing today, knowing the patients I cared for did not get even a fraction of the level of care I would consider acceptable,” one member wrote. Another said simply: “We all struggled to get through the day today.”
The accounts were often harrowing and, as RCN Chief Executive Janet Davies said, “desperately sad”.
But were they powerful enough to advance the debate over safe staffing?
Is anything changing?
Janice Smyth, Director of RCN Northern Ireland, is the College’s lead on safe staffing. “This is a situation that’s not easily fixed – and it’s come about as a direct result of cost-saving measures,” she says. “We have acute shortages of registered nurses all over the UK at a time when research evidence is very clear about the impact of shortages on the quality of patient care and mortality.”
Yet while the experiences of frontline staff may not yet be improving, there are signs of progress.
NHS Improvement, for example, recently published guidance for services in England on safe staffing in five areas, adding to earlier guidelines on urgent and emergency care, and maternity services.
And the Scottish Government is developing a bill on safe staffing, expected later this year, following a commitment by First Minister Nicola Sturgeon at RCN Congress 2016. The RCN is working hard to ensure the bill is fit for purpose.
The bill needs to do far more than just put the status quo into legislation
Rachel Cackett, RCN Scotland Policy Adviser, says discussions with the team drafting the bill are ongoing, and the RCN has seats on all the groups influencing it.
“We’re doing everything we can to ensure those writing the bill understand our perspective and what needs to be included to make a real difference to our members. As always, the devil will be in the detail – and we’ve not seen that yet.”
NHS boards had already been directed to use NHS Scotland’s workload and workforce planning tools, but these are not resulting in the right workforce being in place to meet patient need, says Sian Kiely, RCN Scotland Knowledge and Research Manager.
“The bill needs to do far more than just put the status quo into legislation. So we’re lobbying on lots of issues, from making sure the role of the senior charge nurse or team leader is non-caseload-holding to ensuring the bill has real teeth if care isn’t safe because of too few staff.”
Clearly workforce planning goes hand in hand with safe staffing – or it should
Janice says: “Across the four countries of the UK, there are issues about identifying clearly who is responsible for developing workforce strategy and commissioning pre and post-registration education. Things are not as clear and robust as they should be.
“We know, for example, that in Northern Ireland there was no workforce planning done between 2009 and 2015, and during that period decisions were made to cut the number of nurses being trained.”
This continuing depletion of nursing numbers in a bid to save money is a false economy, she says.
“Agency bills are soaring and not having enough staff impacts the wellbeing of patients. But there is now also evidence that it is adversely impacting the health and wellbeing of nurses. Sickness absence rates are at an all-time high.
“So we contest very strongly that the actions taken have saved money. We don’t accept that it’s costly to provide an appropriate level of registered nurses – we believe it’s very costly not to.”
A graphic example of the effect on staff wellbeing of nursing shortages came recently in a letter to the RCN from member Karen Summers.
Karen was a ward sister, a job she was passionate about, but which she left because of the despair she and her team felt about being able to provide only minimal standards of care.
Every day is like the aftermath of a major incident
"If you chip, chip away at a large establishment such as the NHS over a long period, the effects of these cuts may not immediately be obvious and therefore may be absorbed and go unnoticed. Then, all of a sudden, as we are witnessing now, the whole ship starts to rock, take on water and many (such as me) will jump before they drown," she says.
"Every day is like the aftermath of a major incident. Staff are moved, sometimes twice in one 12-hour shift, in an effort to try and keep staffing levels above at risk. Those that don't come to work fearful or in tears will surely go home crying."
In Wales, however, there are grounds for cautious optimism
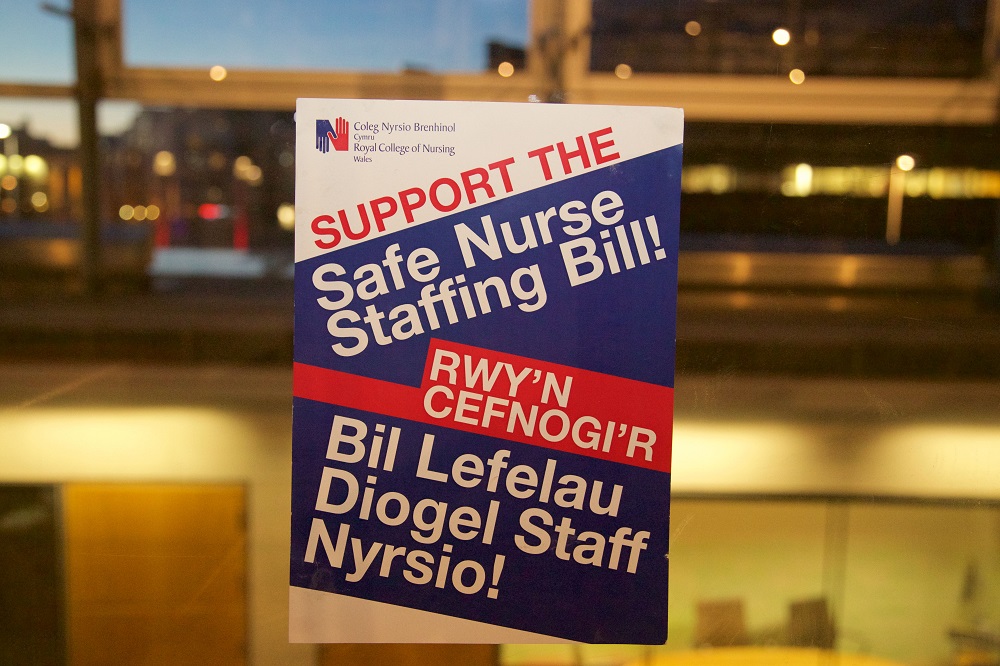
The Nurse Staffing Levels (Wales) Act became law in 2016, with a phased implementation. Its purpose is to ensure NHS organisations are providing sufficient nurses to allow sensitive care for patients.
“We were very pleased that the Welsh Government supported the passage of the legislation," says Tina Donnelly, Director of RCN Wales.
"This is the first time in any part of the UK that the NHS has legislation that focuses upon legal accountability for the delivery of safe nursing care. It takes into account numbers of qualified nursing staff, the ratio of registered nurses and support staff and the skill mix,” Tina says.
“We’re also delighted that the Government accompanied it with a significant increase in the commissioning of student nursing numbers for the last two years, as we believe this is needed to deliver safe care.
“At the same time, our role is to look after the interests of our patients and members, so obviously we’re going to be scrutinising the health boards in the delivery of the requirements of the legislation.”
And as Lisa Turnbull, RCN Wales Policy and Public Affairs Adviser, is keen to emphasise, there is more to safe staffing than new laws. “Legislation is a huge step forward but it is not the be all and end all. Safe nursing care also requires funding, cultural changes, changes to processes and ways of working. There are lots of aspects to this we need to watch. But at the same time, when we see successes we want to extend them.”
‘The act will empower nurses’
RCN member Joanna Doyle manages the All Wales Nurse Staffing Programme, which supports NHS Wales to fulfil the requirements of the Nurse Staffing Levels (Wales) Act. She says:
“Health boards are formulating operational and strategic plans to ensure they have local processes and procedures in place to calculate and maintain nurse staffing levels, in accordance with the act. The level of engagement and support for the national programme of work is to be commended. Nursing staff and students recognise the value of the work and welcome the opportunity to be involved.
“It will be the priority and a legal requirement for every health board to comply with the act, albeit in the face of a shortage of nurses, financial pressures and limited resources. It’s acknowledged that despite resources being limited, health boards are responsible for ensuring resources are allocated efficiently and effectively to meet the requirements of the act.
“The act will empower nurses, providing them with the evidence they need to support their professional judgement when determining the nursing workforce required to meet the needs of patients. And it will provide them with mechanisms and support in cases where they have concerns regarding nurse staffing levels.”
Find out more
Safe staffing means having enough nursing staff with the right skills and knowledge, in the right place, at the right time.
Without safe staffing levels in place, nursing staff are struggling to provide patients with the safe and effective care they would like to, and which patients deserve.
The RCN plans to launch a campaign for safe and effective staffing levels in each country of the UK in the coming months.
Find out more about this work and how to get involved on the safe staffing pages of the RCN website.








