One hundred years ago, at least 50 million people died as a result of the influenza pandemic. Today flu remains a threat as an acute viral infection that can spread rapidly among people who are in close contact with each other – especially during winter months.
Times have moved on, but since the 1960s the flu vaccine has become an integral part of helping to prevent the spread of the infection, by vaccinating those most at risk of contracting it, or more likely to pass it on to others.
Nursing staff have a duty of care to their patients, and flu vaccination for health care workers with direct patient contact is fully supported by professional bodies like the RCN and British Medical Association (BMA).
The RCN recommends all members are fully vaccinated as part of their professional responsibilities to reduce the risks of spreading the infection to the people they care for.
Yet there are still many nursing staff who aren’t coming forward for vaccination, despite employers offering the vaccine free of charge and the good safety record of the vaccination itself. Although rates have been rising slowing, the numbers vary greatly across the UK.
Protecting yourself
It’s an issue that concerns Lesley Pallett, who’s an RCN safety rep. She wants to encourage all nursing staff to have the vaccination and at Congress earlier this year she asked delegates to consider why more nursing staff aren’t being vaccinated.
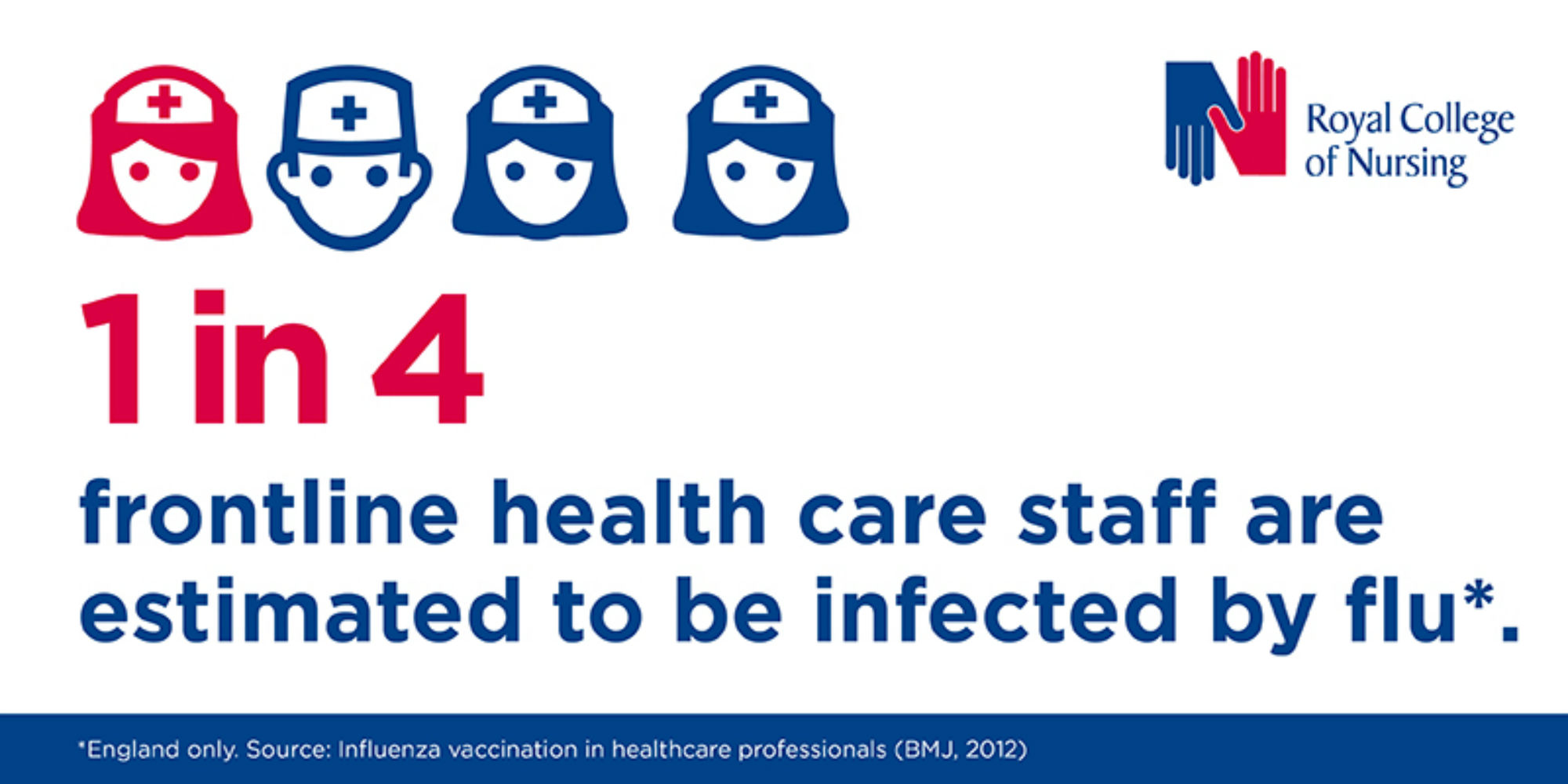
She says: "It’s a really simple way of protecting yourself, and others, against a very nasty virus. If you’ve had the flu you don‘t want to have it again and as a health care worker you wouldn’t want to pass it on to vulnerable patients as you can carry the virus without being symptomatic yourself.
"We need to know how to get the right messages out in the right way to our members, at the right time, to empower them to have the vaccination and for members to be able to get the appropriate message out to those around them."
During the Congress debate Jason Warriner, Chair of the RCN Public Health Forum, said nursing staff need to protect their patients and families.
Helen Donovan, RCN Professional Lead for Public Health, agrees.
“Nursing staff have a professional responsibility to make sure they protect patients and therefore they need to ask line managers or occupational health departments for the vaccine early in the autumn. It takes 10 to 14 days to develop immunity following vaccination, so it’s important to get vaccinated as soon as possible before the flu season really starts," she says.
Ask for the vaccine early in the autumn
The RCN is stressing that it’s really important that trusts make it as easy as possible for staff. Members should also consider the reasons why they cannot have the vaccine, especially if employers move to reserving the right to redeploy them elsewhere.
Helen adds: "A flu pandemic is at the top of the list of threats to the UK. A significant number of people will be infected but showing only very mild or no symptoms. But if you’re infectious you can spread it to vulnerable people. We need to improve the number of people being vaccinated.”