A debate condemning the UK Government’s failure to recognise the impact of its policies on the recruitment and retention of registered nurses was always going to touch a nerve with delegates at RCN Congress.
Members in all areas of health care are familiar with the equation that simply doesn’t compute: consistently safe, effective care can’t be delivered without sufficient nursing numbers.
“Every vacant post poses a risk,” said Mike Smith, a semi-retired emergency nurse who put forward the debate. “Should we be expecting registered nurses to look after 15 high dependency patients on a busy ward for 13 hours at a time?” he asked.
The debate focused attention on a number of factors that have contributed to the current crisis. For example, applicants for nursing courses have fallen following the decision to end the student bursary. And as every RCN member knows, NHS pay policy over the last few years means salaries have failed to keep pace with inflation.
Every vacant post poses a risk. Should we be expecting registered nurses to look after 15 high dependency patients for 13 hours at a time?
But just how serious is the situation? Mike said that in London, where he works, it’s not unusual for trusts to have vacancy rates of 15 to 20%. “There has been virtually no workforce planning in the NHS, with various reactionary pronouncements from Westminster to try and patch up an increasingly fragile service.”
Data from NHS Improvement covering the last three months of 2017 show that the NHS in England had 100,000 vacant positions, of which 35,000 were nursing posts. The shortage of staff contributed to winter pressures, NHS Improvement said, because demand outstripped supply.
In December alone, almost half a million people were admitted to hospital, and in the last quarter of 2017, about 5.6 million people attended A&E – a quarter of a million more than the previous year.
Another challenge is the ageing workforce. A third of nurses are over 50 with many eligible for retirement in the next 10 years. More are now leaving the nursing register than joining, and the number of EU nurses joining the register has fallen by 96% since the Brexit referendum.

Failure to promote nursing as a career choice among younger people is also having an impact across the four UK countries, and delegates at Congress were clear that to ensure a nursing workforce for the future, the UK Government must pay urgent attention to recruitment and retention.
Mike said: “When nurses tell me they sit in their cars in tears because of the pressures and compromises they have in their work, that’s when alarm bells sound for me as an activist.”
He wants to see “robust and long-term” workforce planning to cover the next 10 years, as well as the restoration of training budgets and student bursaries. “We want to hold the Government to account for its action – or rather, inaction,” he said.
'The Government needs to listen'
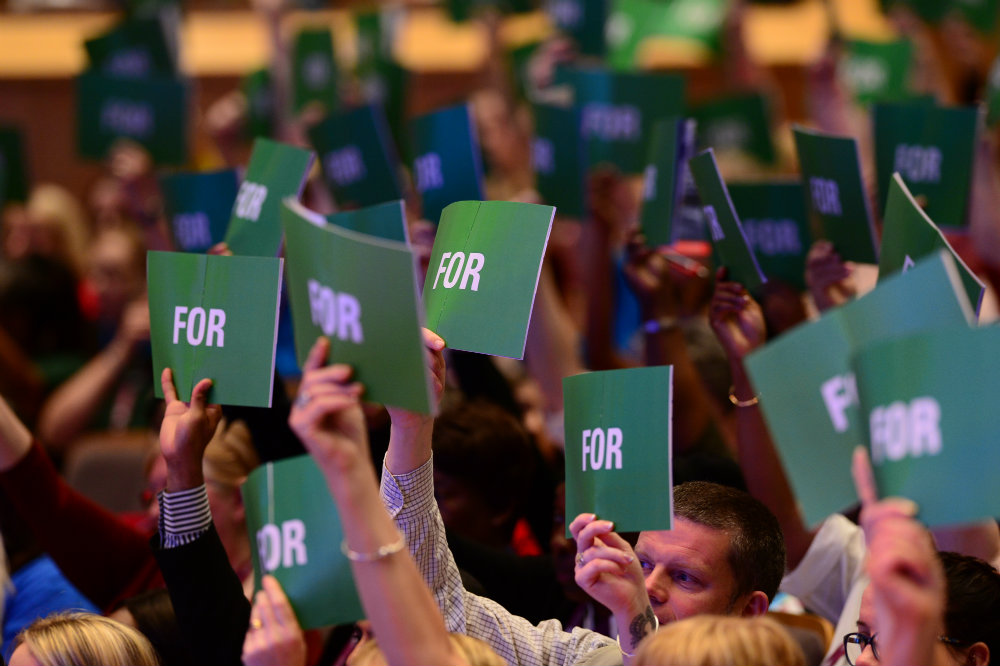
During the debate at Congress, many RCN members shared Mike's concerns and, in an almost unanimous vote, a resolution was passed for the RCN to demand that the UK Government take credible action.
Speaking about the problems her colleagues in the community face on a daily basis, Andrea Wilson, said: "They’re tired, they work with no lunch break, they go home late, they stay over their working hours. We can’t continue. The Government needs to listen."
Cara Large also took to the podium to urge the Government to take note: "I feel that nursing is being eroded with poor staffing levels, poor morale and decreased numbers of new staff. If the Government trust and value nurses as they say they do, they should put their money where their mouth is."
A related debate at Congress focused on the potential risks of redeploying nurses in areas they are unfamiliar with, as employers seek to plug gaps left by local staff shortages.
Providing a move to another area is undertaken with full consultation and appropriate training, any risk is minimised. But anecdotal evidence suggests that nurses who express professional concerns and refuse to move have been threatened with disciplinary action.
The NMC Code requires registrants to acknowledge the limits of their professional competence and not work beyond it, so being moved to another area despite a nurse’s misgivings can pose risks for both registrants and patients.
The debate acknowledged that nurses need to maintain their competence to remain on the nursing register. But when they choose to follow a career in a particular area of care, they may not feel suitably prepared if required to work in a different nursing specialty.
RCN rep Colleen White, who led the discussion, said the problem was particularly acute in Northern Ireland last winter, when sickness and snow exacerbated staffing issues.
“Many nurses were being asked to go and help in other areas,” she said. “And that would be fine if it was just to provide help.” Often, however, they were being asked to take charge of groups of patients within another specialty, which Colleen equates with driving a manual petrol-engine car after years at the wheel of a diesel automatic. “Just because you’re competent in something, it doesn’t mean you’re practised,” she said.
“I raised this as an issue because I want people to start thinking about what they deem acceptable and where you draw a line in the sand. Sometimes it takes a massive incident or crisis before anything is done and I wanted to flag this up before we get to that point.”
Although many people agreed with Colleen that it is important for nurses to raise concerns when they don't feel comfortable working in a certain practice area, the overwhelming feeling in the room was that even if nurses are only providing basic care when working in an unfamiliar environment, it can still make a difference and can help to keep patients safe.
Speaking for the first time at Congress, Natasha Bolt recounted her own experience of working in a busy emergency department with a shortage of staff: “I have been so grateful to nurses who have identified they’re outside of their skill set but they’ve still come and they’ve helped feed patients, they’ve given medication, they’ve rolled patients, they’ve changed pads, they’ve mucked in and they’ve made it more safe by coming.”















