My maternal grandparents lived and worked in the south Wales mining valleys and as a child I was made aware of the local charismatic MP, Aneurin Bevan, and his great achievement: the NHS. The National Health Service was launched in 1948. It has been argued that the model for the NHS was inspired by Bevan’s knowledge of the Tredegar Workmen’s Medical Aid Society, where free health and dental care was available to its members for the payment of a penny a week.

1948 – birth of the NHS
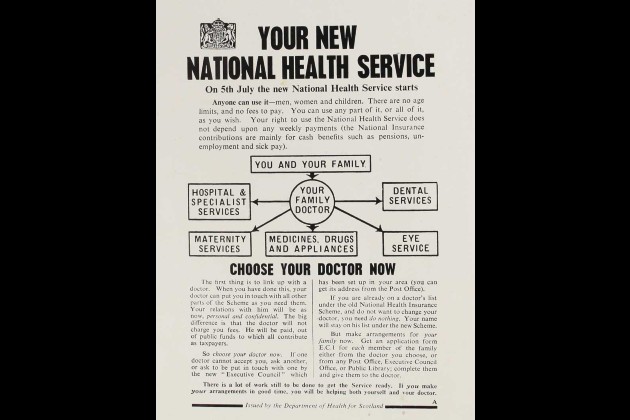
In January 1948, Bevan, then Minister for Health and Housing, announced that on 5 July the National Health Service would launch. In those six months, the introduction of the NHS was resisted in parliament and by doctors and dentists who feared a loss of independence. However, the Socialist Medical Association (SMA) actively campaigned in its favour. RCN member Avis Hutt was a radical activist and member of the SMA. As the implementation date grew closer, community doctors began to advertise for patients and with just five weeks to go, the British Medical Association finally ended its resistance.
1950s – prescription charges and mass vaccination
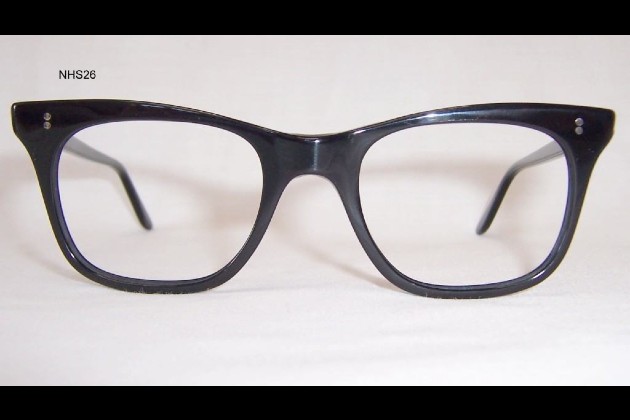
My brother was born just 10 weeks after the beginning of the NHS and my mother was heard to say: “I had to pay for our Dianne, but John came free!” However, that free service only remained truly comprehensive for a short time. The budget of 1951 reduced NHS funding and resulted in Bevan resigning, and in 1952 charges were introduced for prescriptions, spectacles and dental services. There was ongoing underfunding of the service. Nevertheless, health improved, infant mortality reduced, and life expectancy increased. In 1958 the first mass vaccination programme arrived. There were 8,000 cases of polio and 70,000 of diphtheria each year before these vaccinations were offered to all under-15s.
1960s – hospitals for all
Throughout the 1960s – despite long waiting lists, staff unrest over pay and conditions, and a cumbersome bureaucracy – the service continued to have widespread support. The decade saw the creation of district general hospitals. In 1962, Health Minister Enoch Powell’s Hospital Plan set out a vision to build hospitals in every place where there was a population of at least 125,000. Then there was the restructuring of social services and the creation of the Department of Health and Social Security. As a student nurse at the end of that decade, the hospital beds were always full, there was no shortage of equipment or resources, the food for staff and patients was freshly prepared, and much hands-on nursing care was delivered by student nurses. In 1969, the RCN’s Raise the Roof campaign resulted in an impressive 20% pay rise for nurses.

1970s – pay rises for nurses
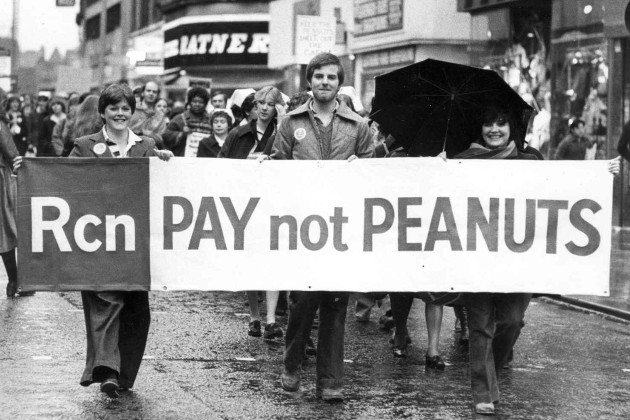
The 1970s have been described as “halcyon days” for the NHS, a time of increased spending and expansion. Yet there were ongoing pay disputes and concern about reforms to the service. In April 1974, the NHS was re-organised with the aim of providing a fully integrated local health service and not everyone was happy with the new layers of bureaucracy. The RCN became increasingly political, nurses pay remained an issue, and the Halsbury Review resulted in an average pay increase of 33%. I was undertaking the two-year sister tutors diploma course at that time. On completing the course and effectively being promoted, I saw a 50% increase in my salary.
1980s – Thatcher’s reforms
The 1980s was a decade of radical change for the NHS, with the introduction of “general management” in 1982 following the Griffiths Report. The Nurses Pay Review Body came into existence after 1983, following an 18-month long pay dispute. At the time, the RCN had a no-strike policy. In the middle of the decade, Project 2000, the first step towards nurse education moving from the NHS to the university sector, was launched and student nurses became supernumerary. The decade ended with social services being split from health at government level, and Margaret Thatcher announcing that there was to be a fundamental review of the NHS: the internal market had arrived.

1990s – new legislation and PFIs
The NHS underwent yet more change during the 1990s, with the introduction of the internal market, NHS trusts, a mental health framework and NHS Direct. The advent of Private Finance Initiatives (PFIs) resulted in an explosion in new hospitals being built, but there were serious concerns about staff employment, as non-NHS contracts were awarded for cleaning and catering services. Devolution allowed for flexibility in spending and organisational structure – there was no internal market in Scotland, while Wales abolished the purchaser/provider split and many hospital-based targets. In 1992, following a successful campaign by the RCN, it became possible for nurses to prescribe medications.

2000s – Agenda for Change
In 2000 the NHS Plan was regarded as the biggest change in the NHS’s history, offering a 10-year reform programme, but in 2004 the NHS England Five Year Forward View arrived. Agenda for Change, the current and hotly debated job grading and pay system for NHS staff, was introduced. The first years of the new millennium also brought us strategic health authorities, foundation trusts, the Care Quality Commission and the NHS constitution.

2010s – nurses graduate
Despite promises of no more top-down change, another significant reorganisation was implemented by the Conservative-led coalition government in 2012 when the Health and Social Care Act was passed. In the same year, nursing finally became a graduate entry profession. In 2017, the nursing associate (NA) role was introduced in England to bridge the gap between HCAs and registered nurses.

2020s – a global pandemic and historic strikes
I was looking forward to celebrating the bicentenary of Florence Nightingale’s birth in 2020. By the time the date arrived, the COVID-19 pandemic had been declared. Pop-up hospitals named for Nightingale were set up to increase capacity. The NHS and its nursing staff bravely facing the dangers of each pandemic wave, dealing with a lack of appropriate medical and protective equipment, dramatic staff shortages, and the deaths and severe illness of colleagues, loved ones, and patients.

Nursing staff were involved in the development of COVID-19 vaccines, helping run clinical trials to test safety and efficacy. On 8 December 2020, May Parsons, a matron at University Hospital Coventry, became the first person in the world to administer a COVID-19 vaccine to a patient outside of clinical trials. The global pandemic has lasting repercussions for the NHS but also led to an overhaul of how services are managed with more trusts using digital resources to care for patients.
After all this, the Conservative government’s below-inflation pay offer to NHS staff frustrated many. In 2022, RCN members in the NHS voted in favour of strike action in all four UK nations. In England, Northern Ireland and Wales members then took historic strike action, withdrawing their labour for the first time on this scale in the RCN’s 106-year history.

The future of the NHS
Yet again the NHS in England is undergoing major change – the Health and Social Care Act (2022) aims to support collaboration and partnership working, and I am reminded of the 1974 re-organisation which had similar aspirations. Time alone will see if a fully integrated health and social care service is delivered.
The NHS continues to experience staff shortages, this has always been the case, but recent strikes by NHS staff have been unprecedented. Despite these challenges I have still been able to access medical advice and guidance. Although I have had to learn new skills to complete online health assessments.
The only real certainty is that the NHS will always be changing, and it will always be subject to political and parliamentary management. But I am confident it will always be defended and defined by its nursing staff.








