The NHS, medicine and British Empire have a long, intertwined history, and sickle cell disorder plays a significant part in that story.
I was always aware of sickle cell, having known people with the disorder, but it wasn’t until I looked at the Black Cultural Archives and began to understand its history that I decided to explore it further.
Sickle cell is an inherited blood condition affecting haemoglobin in red blood cells, giving them an unusual shape so that they can’t pass through blood vessels easily.
Those with sickle cell can present with a host of symptoms which they have to live with for their whole lives. The symptoms are life-affecting and it is a life-limiting condition.
Sickle cell is most commonly found in people who descend from places where malaria has been endemic. It was first identified in the UK in the 1950s, the same time as the first big wave of migration from the Caribbean and Africa and the initial growth of the NHS.
Fuelling fear
There was a considerable amount of institutional racism in the NHS in the middle of the 20th century and, as such, many of the British commonwealth migrants coming into the country were expected to be NHS workers, not patients.
Fuelled by the far-right press in the 1950s and 1960s, there was a feeling that migrants had brought sickle cell into the country. Lack of understanding and unwillingness to learn meant that racist assumptions guided a lot of decisions.
For many years, people believed that sickle cell was an infectious disease that Black people passed on. There was a suggestion made in parliament that Black people should be excluded from donating blood because of the risk of sickle cell making its way into the blood donor stock in the UK.
There was a feeling that migrants had brought sickle cell into the country
Although this never happened, further racist fearmongering attempted to spread the belief that Black nurses in the NHS were passing on sickle cell to their patients.
I’ve spoken to people who were living with sickle cell in the 1960s. Many were too afraid to speak about it to their friends and neighbours, sometimes even keeping it from their own families. I’ve also had the opportunity to interview nurses who worked in the NHS. Although some of them were aware of sickle cell, many were not.

Battling power hierarchies
For many years sickle cell was seen as a niche condition that didn’t affect British people. Patients in desperate need of pain medication were labelled as drug addicts or malingerers, routinely dismissed, abused, or ignored by white health care professionals who didn’t understand the disease.
Many of the Black nurses I interviewed felt that their capacity to intervene was limited. They felt powerless in comparison to NHS policy and bureaucratic decision making.
It's important to remember that at the time, the NHS was even more hierarchical than it is today. Nurses were not respected and faced huge repercussions if they tried to speak out.
Alongside this, many were facing discrimination: the advancement of their own careers was limited because they were Black. They were racially abused by patients and staff and barred from applying for courses that would help them get qualifications or promotions.
Training and development to enable nurses to adequately care for sickle cell patients was non-existent.
Making progress
Over time, things started to slowly change. Networks between medical professionals began to form, providing an understanding of the scale of sickle cell in Britain.
Black nurses got involved in a volunteer capacity, acting as advisers to the Sickle Cell Society or local branches of the Society for Sickle Cell Anaemia. This gave them distance between this work and their roles as nurses and allowed them to provide critique from the outside.
One doctor, who advocated for the Sickle Cell Society, was interviewed on film. She said the reason that sickle cell wasn’t getting the funding or recognition it deserved was because it affected Black people and the NHS doesn’t care about Black people.
Later she asked the filmmaker to take that out because she was afraid of what her employer would do, demonstrating how difficult it was for staff and patients to speak up.
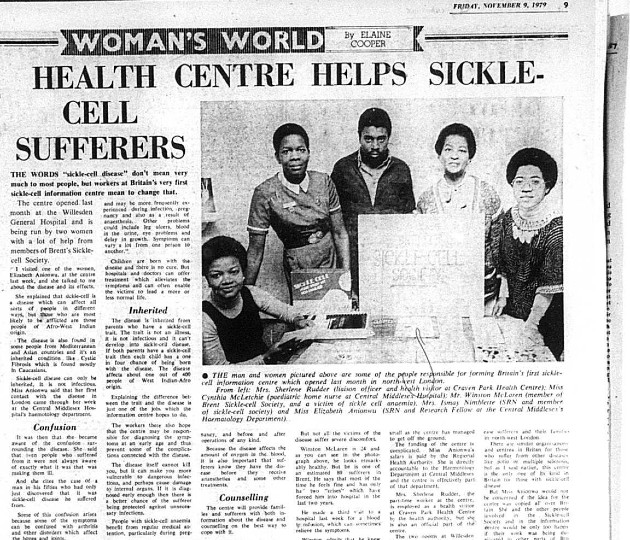
Even when sickle cell services were first set up, they were often run as pilots with limited short-term funding – there was never any guarantee that these services would continue. The health care professionals involved risked delaying the advancement of their careers. It was a real labour of love, but in 1979, the first dedicated centre opened.
The Brent Sickle Cell and Thalassaemia Centre, founded by Dr Misha Brozovic and nurse Dame Elizabeth Anionwu, paved the way for others across the country to specialise in sickle cell and build a strong knowledge-sharing network.
Sickle cell patients were getting the care they needed.
Building on the work of these centres, Dame Elizabeth Anionwu later set up a course to help health care workers offer genetic counselling that is sensitive to ethnic and racial backgrounds. Nurses from all over the country signed up for the training which led to the emergence of nurse consultants and specialists in this area.
For the first time there were groups of professionals, mainly nurses, making sure the right policies and processes were in place and holding people to account.

When sickle cell services were first set up, they were often run as pilots with no guarantee that they would continue
Modern era
Services like the Brent Sickle Cell and Thalassaemia Centre provide patients with a lifeline, allowing them to live as normal a life as possible. However, over the last 10 to 15 years we’ve seen a reduction in the number of specialist services as funding has been eroded.
Things are taking a huge step backwards. Although many established services continue to exist, there is a still a lack of sickle cell training and knowledge in more generalised areas. When patients enter non-specialised areas such as inpatients, A&E or urgent care, they sometimes experience difficulties.
If you are not educated about sickle cell, it can be very confusing to see a patient in sickle cell crisis. They are in a lot of pain, with no apparent organic reason for it.
It’s vital to tackle racist attitudes towards people in pain
Sometimes a person with sickle cell has been living with this pain their whole lives and will have evolved different ways of coping. They may look withdrawn, or they may look normal, so when they say they are in a lot of pain while, for example, scrolling their phone, sometimes they are still not believed.
It’s also vital to tackle racist attitudes towards people in pain, where these continue to exist. There is a lot of information available, so it’s difficult to understand why some patients still struggle to be heard.
To improve patient care now and in the future it’s important that training and funding is available to build upon the institutional knowledge and expertise that currently exists. All health care staff should receive basic training to allow them to recognise sickle cell and provide general care until patients can be moved to a specialist service.
Watch Grace's talk
Historian Grace Redhead, specialist nurse consultant and RCN Fellow Lola Oni, and nurse and sickle cell patient Gildé Nsianguana spoke at an RCN Library event in June 2022 about the history of sickle cell disease and its treatment in the UK.
This event explored the history of sickle cell and race, and the work of healthcare professionals to push for improved health care and better pain management during sickle cell disease crisis.
More information
- Join the RCN History of Nursing Forum
- Read the latest RCN Magazines history features
- Sickle Cell Society
- Brent Sickle Cell and Thalassaemia Centre
- Black Cultural Archives








