Accelerate (2020). Optimising compression - the use of Class 1 hosiery for early intervention.
British National Formulary (2025). Wound management products and elasticated garments.
Clemett, VJ (2025). Wound assessment and documentation: rationale and guidance. British Journal of Nursing, Vol 34, (15), pp S20-S26.
Dowsett C and Hall Y (2019) T.I.M.E to improve patient outcomes: optimising wound care through a clinical decision support tool, British Journal of Nursing, 28(6), pp. S17–S21.
Gray TA, et al. (2018). Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 8(3): e019440. doi: 10.1136/bmjopen-2017-019440.
Guest J, Ayoub N, McIlwraith T, UchegbuI, Gerrish A, Weidlich D, Vowden K, Vowden P (2015) Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 5(12): e009283 - live link - Health economic burden that wounds impose on the National Health Service in the UK - PubMed
Guest JF, Fuller GW, Vowden P (2018) Venous leg ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J 15(1): 29–37 - Live link - Venous leg ulcer management in clinical practice in the UK: costs and outcomes - PubMed
Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 10(12): e045253 – live link - Cohort study evaluating the burden of wounds to the UK's National Health Service in 2017/2018: update from 2012/2013 - PubMed
Guest JF, Fuller GW (2023) Cohort study assessing the impact of COVID-19 on venous leg ulcer management and associated clinical outcomes in clinical practice in the UK. BMJ Open 13(2): e068845 – live link - Cohort study assessing the impact of COVID-19 on venous leg ulcer management and associated clinical outcomes in clinical practice in the UK - PubMed
International Skin Tear Advisory Panel (ISTAP™). Tools and resources for skin tears.
Journal of General Practice Nursing.
Legs Matter (2023). How to treat Varicose Veins – Venous Intervention.
Legs Matter (2024). Can GPNs stop leg ulcers in their tracks?
Legs Matter. Healthcare Professionals. Information for healthcare professionals.
National Wound Care Strategy Programme (2024). Leg Ulcer Recommendations.
NHS England (2024). Decision support tool: making a decision about treatment for varicose veins.
Saliba-Júnior, O. A., Rollo, H. A., Saliba, O., & Sobreira, M. L. (2022). Positive perception and efficacy of compression stockings for prevention of lower limb edema in pregnant women. Jornal vascular brasileiro, 21, e20210101. https://doi.org/10.1590/1677-5449.210101
Skills for Health (2025). A foreword by National Deputy Director, Paul Vaughan: Primary Care & General Practice Nursing Career & Core Capabilities Framework.
Smyth, K (2024) Can GPNs stop leg ulcers in their tracks (PDF). Journal of General Practice Nursing. Vol 10 (3), pp 62-66
Staines K & Mitchell A (2024). ‘Assessment of leg ulceration’ in Mitchell A, Ritchie G & Hopkins A (eds.) Lower Limb and Leg Ulcer Assessment and Management. Chichester: John Wiley & Sons Ltd, pp 226-284.
Vascular Society of Great Britain and Ireland (2018). The Provision of Services for Patients with Vascular Disease (PDF).
Wounds UK (2024). Best Practice Statement: Primary and secondary prevention in lower leg wounds.
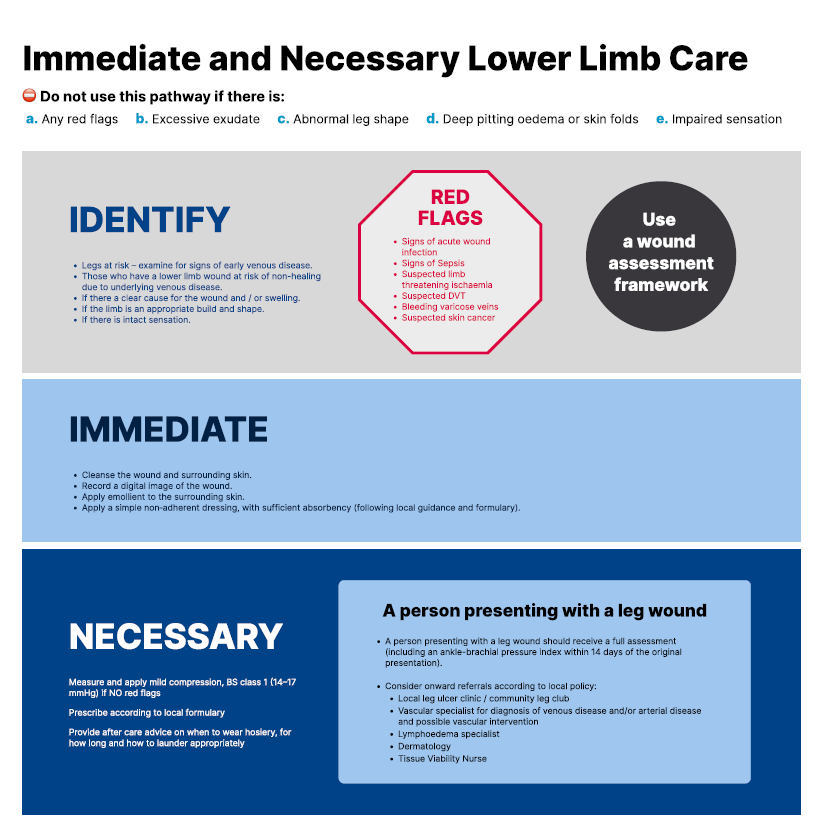
Wounds UK (2023). Quick Guide: Immediate and necessary care for lower limb wounds.
Wounds UK (2022) Best Practice Statement: Holistic management of venous leg ulceration (2nd edition).
Wounds UK (2021). Best Practice Statement: Compression hosiery: A patient-centric approach.
World Union of Wound Healing Societies (2016). Position Document. Advances in wound care: the Triangle of Wound Assessment (PDF).