UK Career Framework For Stroke Nurses
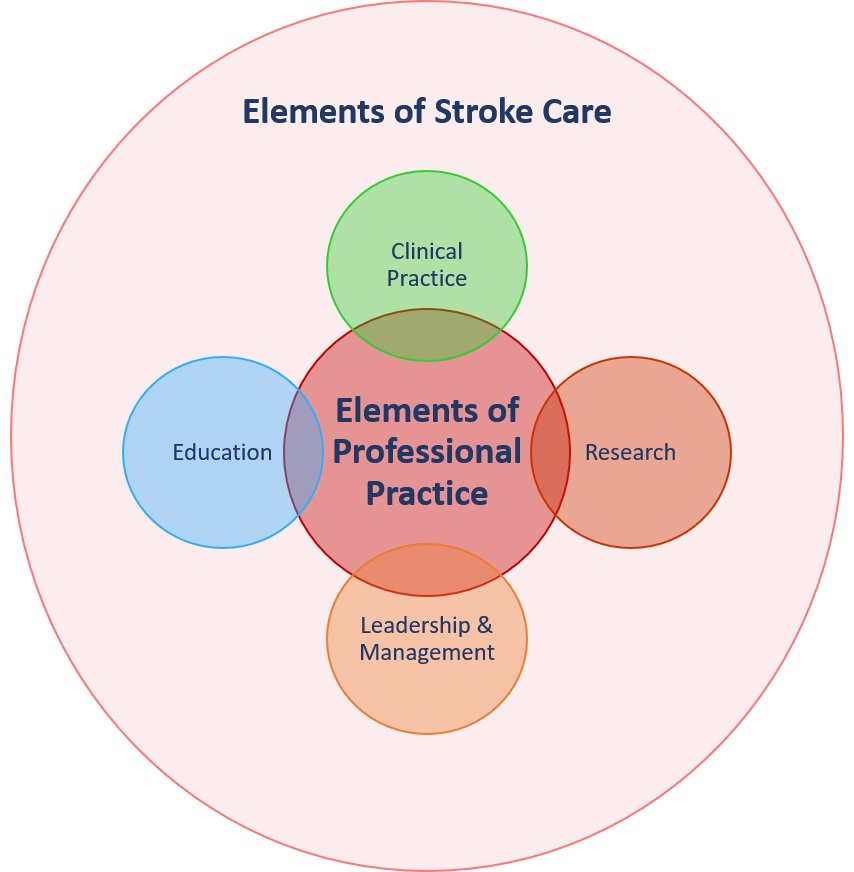
The UK Career Framework for Stroke Nurses showcases the range of career pathways within stroke nursing. This framework is intended to guide the development of the stroke nursing workforce of the future. Discrepancies between this framework and current practices are expected across the UK. Despite this, we recognize that individual and organizational efforts should focus on channelling resources and creating the necessary structures to move beyond these differences, for the benefits it brings to patient care.
The UK Career Framework for Stroke Nurses does not intend to be linear or prescriptive but to demonstrate the range of opportunities that registered nurses working within stroke care can consider in their career development. Transition between pathways is possible and, therefore, practitioners can consider exit points in a different pathway. In addition, employers may also opt to combine roles to answer the specific needs of patients and services in their local areas. For instance, the role of a Senior Staff Nurse/Deputy Charge Nurse (in the Clinical Practice pathway) may be combined with a Practice Assessor role (in the Practice Education pathway); a Clinical Nurse Specialist / Advanced Practitioner – Stroke (in the Clinical Practice Pathway) may also be a Clinical Academic Training Fellow (in the Clinical Academic Research Pathway). In such cases, it is fundamental that educational requirements for both roles are taken into consideration.
The role titles in this Framework have been aligned to the RCN definitions of levels of practice. This is in attempt to consolidate existent variations within the stroke nursing and the wider nursing profession. Due to Agenda for Change banding variations and varying use of job titles, it is essential that priority is given to the description of each role, the level of practice, and the recommended education requirements. These define best the scope, knowledge and skills of the practitioner. Education requirements are recommended as an entry point or completion in each post.
We recommend that stroke nursing workforce career development plans and strategies in each stroke service are aligned with this framework. This framework should be used in conjunction with the Stroke Specific Education Framework and aligned with the National Clinical Guideline for Stroke.

 NHS Long Term Plan (England)
NHS Long Term Plan (England)