UK Career Framework For Pain Nurses
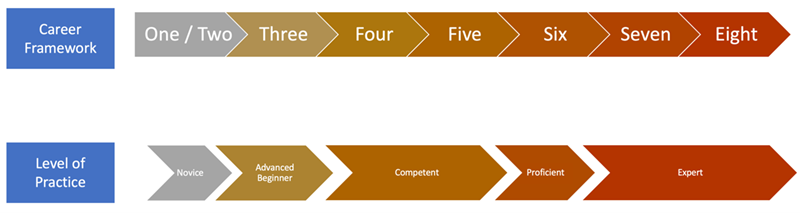
The UK Career Framework for Pain Nurses showcases not only the range of career pathways within pain nursing but also outlines the knowledge and skills recommended for each level of practice.
This framework is intended to guide the development of the pain nursing workforce of the future. Discrepancies between this framework and current practices are expected across the UK. Despite this, we recognize that individual and organizational efforts should focus on channelling resources and creating the necessary structures to move beyond these differences, for the benefits it brings to patient care. For this reason, this document has been based on a variety of similar pain related knowledge frameworks in an attempt to standardise practice across the UK.
The UK Career Framework for Pain Nurses does not intend to be linear or prescriptive but to demonstrate the range of opportunities that nurses working within care can consider in their career development. Transition between pathways is possible and, therefore, practitioners can consider exit points in a different pathway. In addition, employers may also opt to combine roles to answer the specific needs of patients and services in their local areas. For instance, a Clinical Nurse Specialist / Advanced Practitioner – pain (in the Clinical Practice Pathway) may also be a Clinical Academic Training Fellow (in the Clinical Academic Research Pathway). In such cases, it is fundamental that educational requirements for both roles are taken into consideration.
The role titles in this Framework are an attempt to consolidate existent variations within the pain nursing and the wider nursing profession. However, it is essential that priority is given to the description of each role, the level (according to the Skills for Health Career Framework) and the recommended education requirements, as these define best the scope, knowledge and skills of the practitioner. Education requirements are recommended as an entry point or completion in each post.
We recommend that nursing workforce career development plans and strategies in each pain service are aligned with this framework.


 Better Health Better Care (Scotland)
Better Health Better Care (Scotland)