
Osteoporosis
What is osteoporosis?
Osteoporosis is a condition in which bones lose their strength and are more likely to break, usually following a minor bump or fall (fragility fractures). Although such fractures may happen in various parts of the body, the wrists, hips and spine are the most commonly affected sites and can significantly contribute to the loss of independence and the development of frailty in older people. NICE has developed a guideline for assessing the risk of fragility fractures (2017).
Who is affected by osteoporosis?
Women are more susceptible to osteoporosis because bone loss becomes more rapid for several years after the menopause, when sex hormone levels decrease. However, one in five men also break a bone after the age of 50 years because of low bone strength. Believing this to be a 'women’s condition', men with osteoporosis tell us that this belief can sometimes make it more difficult to come to terms with the condition and to seek help and support.
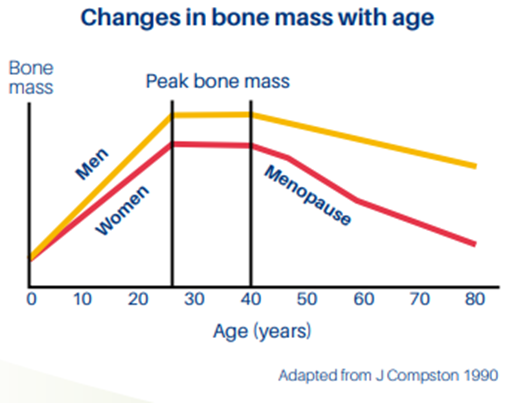
The chart below shows the 'normal' pattern of change in bone mass during a lifetime.
The term osteoporosis is used to describe low bone density as measured on a bone density (Dual energy X-ray absorptiometry (DXA) scan and compared to the young healthy adult average. This means bones may have lost strength.
In practice, osteoporosis may also be diagnosed when someone, usually post menopause or in later life, has non traumatic spinal fractures with no underlying pathology in association with other risk factors. Risk factors include non-modifiable factors such as old age, female gender, low body weight and others which may be modifiable such as immobility, excessive alcohol smoking and falls risk. Medications such as glucocorticoids and some breast cancer and prostate cancer treatments and other medical conditions such as rheumatoid arthritis also increase fracture risk. See: all NICE guidance, advice and quality standards on osteoporosis.
Osteoporosis drug treatments are prescribed for adults where there is a high risk of fragility fractures. Guidance from UK experts has been developed to support their use in accordance with NICE guidance, (NOGG 2021). Guidance is also available from NHS Scotland (SIGN 2021).
Adopting a healthy, active lifestyle and minimising known risk factors can help people to look after bones and maintain bone strength. The Royal Osteoporosis Society in partnership with clinical experts, have developed guidance on exercise and osteoporosis and nutrition for bones, including calcium.
Rare types of osteoporosis
- Idiopathic juvenile osteoporosis is a rare condition in which broken bones occur in children following minor levels of trauma, without an apparent underlying problem.
- Pregnancy associated osteoporosis is a rare condition when bones break easily, usually in the spine, or occasionally the hip, around the time a woman is giving birth, causing pain and disability. They may also occur 8-12 weeks following delivery. Maternal age is not a risk factor and although more common in first pregnancies, it can sometimes occur in subsequent pregnancies after a normal first pregnancy. It is unclear why this happens. Broken bones heal in the normal way and usually women recover fully. However, when bones break it can be frightening and confusing for the women affected, and their families.
- Complex Regional Pain Syndrome (CRPS) and Transient Migratory Osteoporosis are related bone conditions which may sound similar to osteoporosis, or share causes, symptoms or treatment options.
Vitamin D
Vitamin D is essential for musculoskeletal health since it promotes calcium absorption from the bowel, promotes mineralisation of bone and supports muscle function. Following the Scientific Advisory Committee on Nutrition (SACN) vitamin D and health report (2023), Public Health England recommends that everyone over the age of one year should get 10 micrograms or 400 IU (international units) every day. This is to top up the vitamin D received by exposure to sunlight. Daily supplements are recommended for those at risk of deficiency and to be considered by everyone during the winter months.
Guidance developed by the Royal Osteoporosis Society on Vitamin D and bone health (PDF) in adults identifies that adults at risk of vitamin D deficiency include:
- Older people > 65 years
- People who have low or no exposure to the sun, for example those who cover their skin for cultural reasons, who are housebound or who are confined indoors for long periods
- People who have darker skin, for example people of African, African-Caribbean or South Asian origin, because their bodies are not able to make as much vitamin D
- It is recommended that people aged > 65 years and those who are not exposed to much sun should also take a daily supplement containing 10 μg (400 IU) of vitamin D.
Osteoporosis statistics
Fragility fractures
- One in two women and one in five men over the age of 50 are expected to break a bone in their lifetime (Vanstaa TP et al 2001)
- The number of incident fractures predicted in 2025, taking into account demographic projections, has been estimated at 682,000 in the UK. This represents an increase of 146,000 fractures from current levels (Svedbom A 2013)
- It is estimated that every year in the UK there are more than 500,000 fragility fractures, that’s one every minute (1,400 a day). (Svedbom A, et al 2013)
- One in three people with long term pain after fractures describe it as “severe” or “unbearable” (NOS 2021)
- More than 3 million people in the UK are estimated to have osteoporosis (Svedbom A 2013).
Hip fractures
- Hip fractures alone account for 1.8 million hospital bed days and £1.1 billion in hospital costs every year, excluding the high cost of social care. (GOV.UK 2021)
- "1 in 4 people (28.7%) die within a year of suffering a hip fracture” (Neuburger, et al 2015).
Vertebral fractures
- There are currently 66,000 vertebral fractures each year and 50 – 70% of these are undiagnosed." (NICE TA161 2008)
- 58% of people who have experienced spinal fractures are in long-term pain which they don't think will ever go away (NOS Life with Osteoporosis, the Untold Story).
References
Donaldson, LJ et al (2008) The epidemiology of fractures in England. J Epidemiol Community Health, Journal of Epidemiology and Community Health 62(2):174-80
Leal et al (2016) Impact of hip fracture on hospital care costs: a population-based study Osteoporosis International 2016;27:549–58
National Osteoporosis Society (2014) Osteoporosis: the untold story
Neuburger J, et al (2015). The Impact of the National Clinician-led Audit Initiative on Care and Mortality after Hip Fracture in England. Med Care. 53(8): 686–691
NICE (2008 updated 2018) TA 161 Raloxifene and Teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women
Svedbom A (2014) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos. 8(1-2):137
Osteoporosis professional resources
Find out more about Osteoporosis professional resources, including guidance and tools and support from the Royal Osteoporosis Society.
Pregnancy Associated Osteoporosis
Pregnancy Associated Osteoporosis (also known as Pregnancy and Lactation Osteoporosis) is a rare form of osteoporosis, which affects pregnant or postpartum women. It is associated with frail bones that fracture with little or no trauma, particularly in the spine, causing debilitating back and/or hip pain and related complications.
The Pregnancy Associated Osteoporosis group are an expert patient group and have collated a series of Frequently Asked Questions (PDF) on this topic.
Pregnancy Associated Osteoporosis UK is a charity dedicated to supporting those affected by Pregnancy Associated Osteoporosis for patients and health care professionals.
Page last updated - 08/10/2025





